 What is knee arthritis?
What is knee arthritis?
There are over 100 different kinds of arthritic conditions that affect humans. The word “arthritis” literally means “inflammation of a joint”. Osteoarthritis is also called degenerative joint disease, and is the most common form of arthritis. It is an age related wearing out of the smooth cartilage surface that covers the bone ends at a joint. There is a hereditary form of osteoarthritis (your parents passed it to you in their genes!). Also common is a post trauma form which results from previous injury to the joint. Arthritis causes PAIN.
Why does my knee hurt?
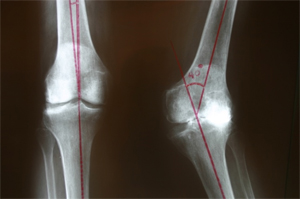
As the smooth cartilage wears away, the bones grind together, which causes irritation, particle release, fluid formation, swelling, and stiffness. At early stages, simple anti-inflammatory medication like aspirin or Motrin can limit symptoms. The arthritic knee may become deformed – the most common deformity is varus or bowleg. It can also become a flexed or knock knee deformity as in Figure 1.
Why does my knee hurt?
As the smooth cartilage wears away, the bones grind together, which causes irritation, particle release, fluid formation, swelling, and stiffness. At early stages, simple anti-inflammatory medication like aspirin or Motrin can limit symptoms. The arthritic knee may become deformed – the most common deformity is varus or bowleg. It can also become a flexed or knock knee deformity as in Figure 1.

What is a Total Knee Replacement?
Watch this video introducing our new website to Total Knees (click here)
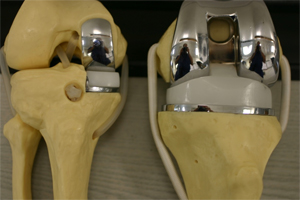
The cartilage on the ends of the knee bones (femur and tibia) are surgically removed and replaced by smooth metal (titanium) and plastic (cross-linked polyethylene) surfaces which have no nerve endings, and therefore eliminate pain. There is a plastic button which is cemented to the undersurface of the knee-cap. There are different design types of total knee replacement. Both fixed bearing knees, and rotating platforms exist. Your surgeon will explain certain advantages of each type.
What is a Partial Knee Replacement?
A partial knee is also called a uni knee replacement. It is a smaller operation that only replaces on side of the knee joint. Only 25-30 % of arthritic knees can be appropriately treated with a partial knee. A big advantage of partial knees is a smaller incision and a much more rapid recovery period. Dr. Kozinn is a world renowned expert on partial knee replacement!
What are the long term results of Total Knee Replacement?
Results are excellent in the vast majority of patients, (reports are as high as 98% short term success), but complications can occur. Some patients with Total knees will still have some pain and mild swelling with over-activity, but the pain is usually much less than before surgery. Typical results show 80% of total knees will still be functioning after twenty years of good use. The rest may need revision at any time because of possible cement loosening, plastic wear, or stretching of ligaments -which can cause symptomatic instability.

What are the possible short term complications of TKR?
All surgeries carry some risk of complications. As with any surgery, there is a small risk of infection (1%). Blood clots in the vein of the leg can occur (1.5% in my patients). Rarely a clot can travel to the lungs (.2%). The rare but possible death rate from knee replacement is quoted to be about 1 in 8,000 ( possible cardiac, stroke, or pulmonary embolism).
If my knee implant fails, can it be replaced?
Yes, revision knee replacement is very successful. Many of my patients tell me their revision knee feels better than the first knee that they had! Special implants with metal stems and metal augments are available to make up for areas of weak bone or bone loss. Recovery is similar to primary total knee replacement. This is the major reason we no longer make younger patients suffer until they can’t stand it anymore.
Am I too old (or too young) for knee replacement?
Age alone is not the deciding factor. There is no upper age limit for a patient that is otherwise healthy, as the risks are more related to general medical condition.
Younger patients are having joint replacement, as the results are better and more long lasting. I will try to hold off on patients younger than 40, but if the joint is bone on bone, than knee replacement is usually still the best option. New cross-linked plastics are hopefully going to extend the life of modern knee replacements, possibly to thirty years. All of my patients are walking in the hospital by 2 hours after the surgery!
Do you do minimally invasive knee surgery?
Yes when it is indicated. But the technique is not only measured by the length of the skin incision. It has to do with sparing as much muscle under the skin as possible during the implantation to decrease pain and speed recovery. It has been proven that if you try too hard to work through an incision that is “too small”, the results of knee replacement suffer. The best option is to let the surgeon choose the approach at the time of surgery that best treats your disease and maximizes your recovery.
When do I know my pain is bad enough to have a knee replacement?
Every patient is different, but when you have pain with every step, and you take pain pills, you are ready to consider it. Younger patients are usually concerned about missing work, or taking care of other family members. Usually, with planning, all of these issues can be worked out. Patients can usually return to desk work or light duty jobs by two weeks post op. If the left knee is done first, patients can drive their car within a week.

What is the best way to insure a rapid recovery?
Choose an experienced surgeon. It is OK to ask how many he or she does in a year. We work in a comprehensive “Total Joint Center” which utilizes a team approach to making our patients well. A positive attitude helps immensely. My patients get a “femoral nerve block” pre-op that eliminates much of the pain after surgery for 36 hours, which allows for a quicker recovery. A physical therapist will help you regain your range of motion post-op.
Will I need a blood transfusion?
The vast majority of patients do not need a blood transfusion, and so we do not recommend pre-op donation of blood. In some cases, a drain is placed in the knee, and the blood collected from it can be re-infused in to the patient if needed. A tourniquet is used on the thigh for about one half of the case, which also decreases blood loss.
Will I need special equipment?
The hospital will supply crutches or a walker as needed, however you may bring your own if you have any. Your health insurance usually pays for these things as part of the hospitalization. We NO LONGER USE a CPM machine at home (constant motion) as all studies on it have found no additional benefit in regard to final results. we will sometimes use it during the two day hospital stay to help desensitize the knee during early motion.

Will I go home or to a rehab facility after surgery?
MOST patients should go home. The knees are fairly indestructible and your home is actually less likely to harbor any harmful bacteria than a rehab or nursing facility. home help can be arranged as needed. We prefer outpatient PT as it leads to better results than home therapy. It is also important to “get out of the house”, which is an important form of therapy in itself. If you live alone with no help available, a rehab facility or nursing home can be arranged by social service in the hospital.
What will my restrictions be after surgery?
You are limited by your pain only. I encourage my knee patients to do as much activity as they can. Sometimes swelling will limit how much you can be up and about, and in that case you will have to decrease that activity for a while. unlike hip replacement surgery, where PT is not essential, most knee patients will go to PT 3 times a week for 4 to 6 weeks. It is important to have some help to regain full knee range of motion.
How long before I am completely healed?
I tell patients that their knee continues to improve for an entire year after surgery. At ten weeks post-op most patients are back to most of their normal activities, including golf. Tennis may take a month more. Some people heal slower than others. Remember, knees and their owners come in many sizes and have different personalities (see figure 6). Most patients stop taking all narcotic pain meds about 4 weeks after surgery.

When will I be seen again after surgery?
You come back to the office for a wound check at 10-14 days. At that visit, the sutures are sometimes ready to be removed. Otherwise you will come back a week later to get them out. Next visit is usually a month later. You will be put on a blood thinner to prevent clots for about 30 days. Recently, most patients have been put on Aspirin twice a day, and our results are equivalent or better than using the more potent Coumadin or Lovenox. High risk patients for clotting ( eg: those with a previous history of clotting) may be put on injectable Lovenox or Coumadin instead.
Please watch this amazing video of Michele’s journey out of a wheelchair after bilateral total knee replacements!
Where can I get more information?
Please come in for an appointment and we will educate you further. We have a large binder filled with useful information to give you. Our Total Joint center at Scottsdale Osborn gives a weekly free class in what to expect with TKR every Thursday. If you call us, we can reserve a spot for you to learn more. You do not have to commit to having surgery to attend these classes. If needed: Search the web by typing “Total Knee replacement” into Google and read the thousands of articles and videos that come up! Brian Williams from NBC News is having a Total Knee. Watch his video from NBC Nightly news about it here.









