What is the Societal Value of Total Knee Replacement?
TKA study is first of a series to identify the value of orthopaedic procedures to society
With all the attention on the cost of health care, an important factor is being overlooked: the impact on society resulting from the treatment of a particular condition. Comparing that impact when both surgical and nonsurgical treatments are available is particularly important in a specialty such as orthopaedics, which focuses on restoring mobility and health.
“A number of studies have already looked at the cost-effectiveness to individual patients for certain orthopaedic procedures, including total hip and total knee replacement ,” said AAOS Past PresidentJohn R. Tongue, MD. In outlining the goal behind “The Direct and Indirect Costs to Society of Treatment for End-Stage Knee Osteoarthritis,” a study published in the Aug. 21 issue of the Journal of Bone & Joint Surgery, Dr. Tongue noted, “We wanted to examine the cost-effectiveness of orthopaedic procedures from a societal point of view.
“For example, if you’re a 55-year-old teacher and you need a total knee arthroplasty (TKA) to keep teaching, and you undergo the procedure, you’re going to continue to work; you’re going to continue to pay taxes. If you don’t, you’re more likely to sit around, developing other comorbidities, gaining weight, having poor quality of life, and collecting disability.”
Applying a new model
Inspired by published research that attempted to quantify the societal impact of deaths and injuries from roadway trauma, Dr. Tongue contacted an economist friend to see if it might be possible to similarly quantify the impact of orthopaedic procedures.
“The gold standard for this type of research,” explains Dr. Tongue, “would be a randomized, prospective, double-blind study with long-term follow-up, but that’s not logistically or financially feasible.”
The economist, John Duffield, PhD, proposed conducting a literature search to identify previous work that may have covered similar ground, then building on that research to develop a new methodology that could be applied to specific medical conditions. To carry out this objective, AAOS engaged KNG Health Consulting, LLC, and its research partners at IHS Global, Inc., and Duke University.
“We developed a three-step process,” explains Lane Koenig, PhD, of KNG Health. “The first step used data from the National Health Interview Survey to estimate the relationship between functional limitations and economic outcomes.
“In the second step, we collected or obtained data that showed how functional limitations are affected when someone has a particular surgical treatment. With those two bits of information, we estimated the change in economic outcomes for patients who underwent surgery and for those who didn’t have surgery,” he continued. “Finally, we entered that data into a Markov decision model, which enabled us to model lifetime costs and benefits of TKA.”
A Markov model enabled the researchers to account for a variety of potential outcomes. Although most patients who undergo TKA may have good results, a certain percentage may require revision surgery or experience some other negative outcome, including—potentially—death. The Markov model offered a validated approach to estimate the impacts identified by the study—an important consideration in any research—but even more critical in a study that Dr. Tongue anticipates will be carefully reviewed by payers and policymakers.
“One of the legitimate concerns raised when we began discussing possible methodologies with AAOS committee members was to be certain that conclusions represent quality science,” Dr. Tongue explained. “We believe we have done a good job with that. The first publication spells out the methodology in a peer-reviewed economic journal, Cost Effectiveness and Resource Allocation. That paper outlines the methodology and makes it available to other researchers for examination and discussion, and application to other health conditions.”
$12 billion in savings
To estimate the societal value of TKA, the research team generated Markov model results based on adults age 40 years or older who underwent TKA during 2009. According to the authors, the study population accounted for 99 percent of all TKAs performed in the United States that year.
The researchers calculated direct costs, quality-of-life, and most importantly the lifetime indirect cost of TKA. These indirect costs components capture the effects of surgery on a patient’s ability to work, patient earnings, disability payments, and missed work days. For modeling purposes, the researchers conservatively assumed that all patients retire at age 75.
The research team found that, compared with nonsurgical treatment, undergoing TKA increased direct costs per patient by an average of $20,635 (based on 2009 dollars). Those costs were offset by societal savings of an average $39,565 per patient based on reduced indirect costs, producing an estimated $18,930 in lifetime savings to society per patient.
Overall, the researchers found that 85 percent of the societal savings were associated with increased employment and earnings. The remaining 15 percent were linked to fewer missed work days and lower disability payments.
Based on the more than 600,000 TKAs performed in the United States during 2009, the study authors estimated a lifetime societal savings of approximately $12 billion for the single year studied.
“When we submitted the study, there was some concern among reviewers that the findings could be interpreted as, ‘everyone should get surgery,’” said Dr. Koenig. “It’s important to understand that is not the conclusion of the study. The conclusion is that, for the cohort of people who have surgery, there are—on average—societal savings. For many reasons, some patients don’t undergo surgery. Our analysis was based on the cohort of patients who actually underwent surgery.”
Further research
The TKA study is the first of five similar research papers planned for publication, each examining the value of a different orthopaedic procedure.
“We chose a variety of conditions based on high economic impact and to demonstrate the breadth of our specialty,” said Dr. Tongue. “We have already submitted for publication papers on rotator cuff repair and anterior cruciate ligament repair, and two more studies—one looking at hip fracture and one on lumbar diskectomy—are in the works. We’re also looking into the possibility of teaming with orthopaedic specialty societies to use the methodology that was developed to examine the value of additional procedures.”
According to Dr. Tongue, the study methodology allows expansion beyond the original five procedures. Several specialty societies have already expressed interest in additional research. In addition, the methodology could be adapted to identify the value of procedures in other countries. In Canada, for example, where the government is both the payer and the insurer, balancing medical costs against societal savings could have an impact on both federal and provincial government budgets.
“What I find most exciting about this research,” said Dr. Tongue, “is that it changes the conversation from how expensive orthopaedic procedures are, to how valuable they are. You don’t have to try to stretch any estimates, because the value for each procedure is tremendous.”
Dr. Tongue’s and Dr. Koenig’s coauthors on the study include David Ruiz Jr., MA; Timothy M. Dall, MS; Paul Gallo, BS; Alexa Narzikul, BA; andJavad Parvizi, MD, FRCS.
Disclosures: This study was funded by the AAOS. Dr. Tongue and Ms. Narzikul—no conflicts. Dr. Koenig— BTG International, Johnson & Johnson. Dr. Parvizi—3M, Cadence, Ceramtec, Pfizer, Smith & Nephew, TissueGene, Zimmer, Baxter, DePuy, National Institutes of Health (NIAMS & NICHD), Stryker, jaypee, Wolters Kluwer Health – Lippincott Williams & Wilkins, American Journal of Orthopedics, Current Opinion in Orthopaedics, International Orthopaedics, Journal of Arthroplasty, Journal of Bone & Joint Surgery—American, Journal of Bone & Joint Surgery—British, Journal of the AAOS, Magnifi Group, Orthopedics Today, SLACK Incorporated, American Association of Hip and Knee Surgeons, American Board of Orthopaedic Surgery, Inc., CD Diagnostics, Hip Society, Orthopaedic Research Society, SmartTech, United Healthcare. Mr. Ruiz, Mr. Dall, Mr. Gallo—no information available.
Peter Pollack is a staff writer for AAOS Now. He can be reached atppollack@aaos.org
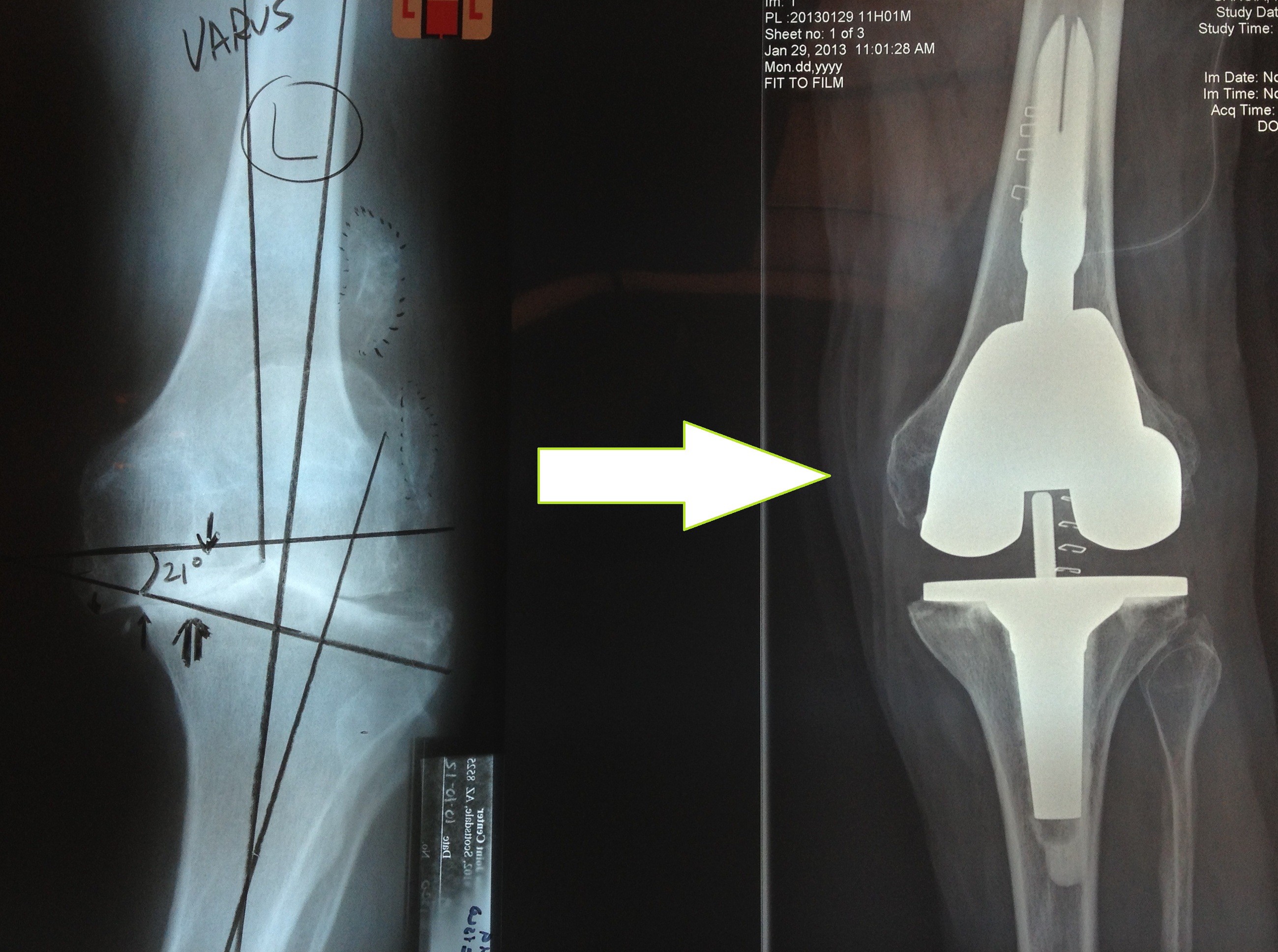
Cover image:
According to the research reported in the August 21, 2013, issue ofThe Journal of Bone and Joint Surgery, total knee arthroplasty delivers positive net savings to society. For more information, visitwww.anationinmotion.org/value/knee
Bottom Line
- Determining the cost benefits to society of specific treatments for musculoskeletal disorders is a new way to demonstrate the value of orthopaedic services.
- This study examined the direct and indirect costs to society for treatment of patients with end-stage osteoarthritis of the knee, based on the 600,000 patients who underwent total knee arthroplasty (TKA) in 2009.
- Compared with nonsurgical treatment, undergoing TKA increased direct costs per patient by an average of $20,635 (based on 2009 dollars)—but net savings to society average $18,932 per patient based on reduced indirect costs.
Additional Resources:
- Modeling the indirect economic implications of musculoskeletal disorders and treatmentDall, et. al. doi:10.1186/1478-7547-11-5
- The Direct and Indirect Costs to Society of Treatment for End-Stage Knee Osteoarthritis JBJS article
- A Nation in Motion press release
AAOS Now
September 2013 Issue
Back Issues of AAOS Now